Preventing Stroke without Medication
Watchman is an alternative to blood thinners for qualified AFIB patients
Heart patient Leonard Williams was 90 years old and determined to continue doing the things he enjoys, such as caring for his acre of property on his riding lawn tractor. That’s why he chose to undergo a preventive heart procedure that would dramatically decrease his risk of stroke and allow him to stop using blood thinners.
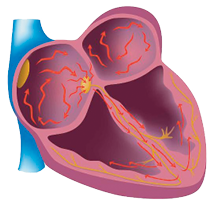
The WWII veteran lives with chronic atrial fibrillation, or AFib, the most commonly diagnosed cause of heart arrhythmia. AFib causes the heart’s upper chambers to beat too slow, fast or irregularly, causing blood to pool and clot. These clots can travel to the brain and cause a deadly or debilitating stroke. “For that reason, stroke prevention is always part of our treatment for AFib patients,” says Waseem Sajjad, MD, an electrophysiologist at the UHS Heart & Vascular Institute.
In May 2017, Dr. Sajjad, along with a team of UHS heart specialists, implanted a Watchman device in Mr. Williams’ heart. Watchman is a screen-and-net-like device that is delivered via catheter, using a minimally invasive approach. It is designed to permanently block off the left atrial appendage to keep blood clots from escaping. The FDA-approved Watchman device is a clinically proven alternative to long-term blood thinner therapy for stroke risk reduction in patients with non-valvular AFib. About the size of a quarter, it is implanted in the left atrial appendage, where 90 percent of AFib-related blood clots collect. Over time, the body’s tissues naturally cover the device, keeping clots from leaving the heart and causing stroke.
The procedure takes one to two hours and is done under general anesthesia. Patients typically remain in the hospital one night and recovery involves healing from a tiny incision in the thigh where the catheter is inserted.
Mr. Williams recovered quickly from the procedure and felt no worse for wear a day later. “It was like going in to get a tooth filled,” he says. “The doctors were amazed how quickly I was back outside.” About seven months later, after visits to the hospital for heart imaging, he was able to stop taking warfarin, a commonly prescribed blood-thinning medication sold under such brand names as Coumadin® and Jantoven®.
Why an Implant?
AFib can increase one’s risk of stroke fivefold. Mr. Williams has watched friends become incapacitated by stroke, and he is very frank about his dislike of that prospect. “I’d rather pass,” he says. Unfortunately, he cannot tolerate the blood thinners that are routinely prescribed to curb that risk in AFib patients.
Blood thinners are effective for many people, but they can cause unwanted side effects in others, explains Dr. Sajjad. In Mr. Williams’ case, they contributed to intestinal bleeding. So he was pleased to discover that the UHS Heart & Vascular Institute, where he receives heart care, is one of the few hospital systems in the region with the expertise and capabilities to offer the Watchman therapy option.
Watchman can reduce stroke risk as effectively as warfarin, the most commonly used blood-thinning drug, Dr. Sajjad says. About 45 days after undergoing the Watchman procedure, 92 percent of patients no longer need to take blood thinners. After one year, 99 percent of patients are off their medication. Watchman has additional benefits. “Unlike warfarin, Watchman can also reduce a patient’s long-term risk of bleeding,” Dr. Sajjad explains. “Most patients no longer have to get regular blood tests and cope with the food-and-drink restrictions that come with warfarin.”
AFIB, AGE and Watchman
Mr. Williams’ advanced age and health history did not prevent him from being a candidate for Watchman, including the fact that he had previously undergone heart bypass and valve replacement surgeries. These surgeries had successfully resolved problems unrelated to his AFib, and he was otherwise healthy and active. This and other factors helped qualify him for the minimally invasive procedure, says Alon Yarkoni, MD, FACC, director of the UHS Structural Heart & Valve Program.
In fact, it’s often older patients who may benefit the most from a medication-free alternative to stroke prevention, Dr. Yarkoni explains. The incidence of both AFib and stroke rise with age, as does the likelihood of being unable to tolerate blood thinners. He notes: “No matter the age, stroke can be incapacitating. That’s why it’s critical that UHS has an experienced, established heart team in place to help ensure the best outcomes for our AFib patients.”
Should I be checked for AFIB?Between two and six million Americans live with AFib, including 9 percent of people over age 65, according to the U.S. Centers for Disease Control and Prevention. AFib can be asymptomatic, but those who do present symptoms may experience one or several of the following:
If you are concerned about possible symptoms of AFib, a primary care physician can perform basic heart function tests to see if referral to a cardiologist is in order. Heart health questions? Use the UHS Find a Provider tool online to find a doctor near you. |